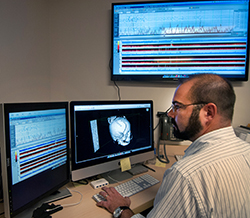
A great deal of information can be gathered to localize the seizure onset zone and important regions of brain function using non-invasive testing such as scalp EEG, inpatient video-EEG, neuropsychological testing, MRI and functional MRI, MEG and magnetic source imaging, PET and SPECT scans. However, in some patients the seizure onset zone can’t be fully defined without direct recordings from the brain.
Pioneers in subdural electrode recording
 Subdural electrode recording for epilepsy is a technique that was pioneered at Washington University in St. Louis. The team at St. Louis Children’s Hospital has a vast clinical and research experience with the technique of subdural electrode recording to map out the seizure focus and critical brain functions in children of all ages.
Subdural electrode recording for epilepsy is a technique that was pioneered at Washington University in St. Louis. The team at St. Louis Children’s Hospital has a vast clinical and research experience with the technique of subdural electrode recording to map out the seizure focus and critical brain functions in children of all ages.
The Pediatric Epilepsy Team at St. Louis Children's Hospital has performed approximately 150 of these procedures in the past decade, with excellent results and minimal complications.
Subdural electrode recording: what to expect
- The child is admitted to the hospital the morning of the surgery.
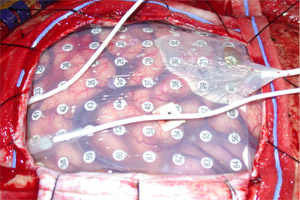
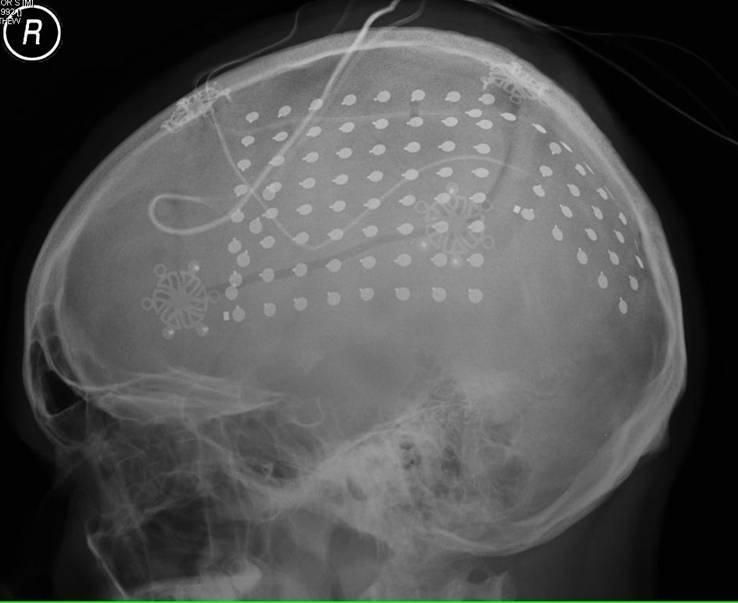
- While under general anesthesia, the neurosurgeon will make a temporary window in the skull, expose the involved area of brain, and lay down specially-tailored electrodes directly on the brain surface, and in some cases, deep in to the brain tissue.
- The temporary bone window is replaced, and the incision is carefully closed.
- The electrode wires come out through the scalp, and the child is then monitored, first overnight in the Pediatric Intensive Care Unit, then on the Epilepsy Monitoring Unit, to capture seizures.
- The dense array of electrodes allows the team to precisely determine the region of brain where the seizures arise. During this period, the child is awake and interacting, just like during a standard scalp Video-EEG session.
- The team may perform cortical mapping to stimulate parts of the brain to identify important areas for movement, sensation and language and their relationship to the seizure onset zone.
- The average course of invasive subdural electrode monitoring is 7 days, but may range from 3 days to 3 weeks.
Selected publications and abstracts from our physicians
- Titus J, Lee A, Kasesbah A, Thio LL, Stephenson J, Steger-May K, Limbrick DD, Smyth MD. Health-related quality of life before and after pediatric epilepsy surgery: The influence of seizure outcome on changes in physical functioning and social functioning. Epilepsy and Behavior, Jun 27;27(3):477-483, 2013.
- Mohammed H, Steger-May K, Kaufman C, Weisenberg J, Munro B, Rothman SM, Grubb R, Limbrick DL, Smyth MD: Impact of epilepsy surgery on seizure control and quality of life: A 26-year follow-up study. Epilepsia 53(4):712-720, 2012.
- Kasasbeh A, Steger-May K, Yarborough C, Limbrick DL, Smyth MD. Characterization of the supplementary motor syndrome after medial frontal lobe resections in pediatric epilepsy surgery. Neurosurgery, 70(5):1152-68, 2012.
- Breshears JD, Gaona CM, Roland JL, Sharma M, Bundy DT, Freudenburg ZV, Zempel J, Limbrick DD, Smyth MD, Smart WD, Leuthardt EC. Decoding Motor Signals from Pediatric Cortex – Implications for Brain-Computer Interfaces in Children. Pediatrics 128(1)e:160-8, 2011.
- Roland J, Miller K, Freudenburg Z, Sharma M, Smyth M, Gaona C, Brehears J, Corbetta M, Leuthardt E. Effect of age on human motor cortical electrophysiology.Journal of Neural Engineering, 8(4):046013, 2011.
- Dorward I, Titus JB, Limbrick D, Johnston JM, Bertrand ME, Smyth MD: Extratemporal, nonlesional epilepsy in children: postsurgical clinical and neurocognitive outcomes. Journal of Neurosurgery: Pediatrics: 7:179-188, 2011.
- Johnston MJ Jr., Mangano FT, Ojemann JG, Park TS, Trevathan E, Smyth MD. Complications of invasive subdural grid and strip electrode monitoring at Saint Louis Children’s Hospital, 1994-2005. Journal of Neurosurgery: Pediatrics, 105:343-347, 2006.
- Schalk G, Miller KJ, Anderson NR, Wilson JA, Smyth MD, Ojemann JG, Moran DW, Wolpaw JR, Leuthardt EC. Two-dimensional movement control using electrocorticographic signals in humans. Journal of Neural Engineering 5:75-84, 2008.
- He BJ, Snyder AZ, Zempel JM, Smyth MD, Raichle ME. Electrophysiological correlates of the brain’s intrinsic large-scale functional architecture. Proceedings of the National Academy of Sciences, in press, 2008.
- Limbrick DD Jr., Kaufman CB, Grubb RL, Smyth MD. Tracing the evolution of epilepsy neurosurgery through the career of Dr. Sidney Goldring. Digital poster presentation to the Congress of Neurological Surgeons, Chicago, IL 2006.
- Johnston J, Smyth MD: CT/MRI fusion for neuronavigation in subdural grid-based epilepsy surgery. Platform presentation to the AANS/CNS Joint Pediatric Neurosurgery Section, Denver CO 2006.
- Schalk G, Anderson NR, Wisneski K, Kim W, Smyth MD, Wolpaw JR, Barbour DL, Leuthardt EC. Toward brain-computer interfacing using phonemes decoded from electrocorticography activity (ECoG) in humans. Poster presentation, Society for Neuroscience, San Diego, CA 2007.
- Anderson N, Wisneski K, Blakely TM, Zempel J, Morrissey M, Smyth MD, Dowling J, Schalk G, Moran DW, Leuthardt EC. Encoding of Target Information recorded using Electrocorticography. Poster presentation, Society for Neuroscience, San Diego, CA 2007.
- Wisneski K, Anderson NR, Blakely TM, Schalk G, Smyth MD, Morrissey M, Zempel J, Dowling J, Moran DW, Leuthardt EC. The Unique Electrophysiology of Ipsilateral Motor Processing and Neuroprosthetic Application. Platform presentation, highlighted abstract, Society for Neuroscience, San Diego, CA 2007.
- Titus JB, Smyth MD, Kanive R, Blackburn LB. Nonlesional extratemporal lobe epilepsy: Neurocognitive outcomes in children after surgery. Poster presentation, American Epilepsy Society, 2007.
- Smyth MD, Titus JB, Dorward I, Kanive R, Blackburn LB. Nonlesional extratemporal lobe epilepsy in children: Post-surgical neurocognitive and seizure outcomes. Platform presentation to the ASPN, Los Cabos, Mexico, 2008.










