What is Congenital Diaphragmatic Hernia (CDH)?
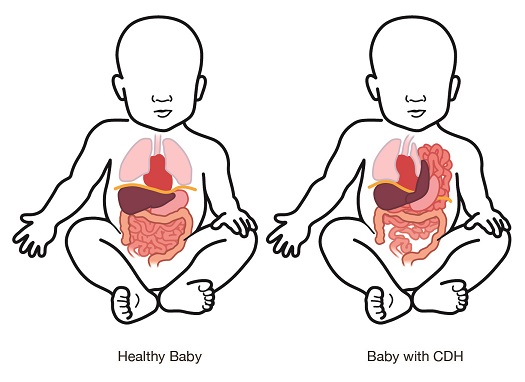
Congenital Diaphragmatic Hernia (CDH) occurs when the thin muscle that separates the lungs from the abdomen fails to close. This hole in the diaphragm muscle allows the abdominal organs to move into the chest. This may include your baby’s intestines, stomach, and possibly the liver. This makes it difficult for your baby to breathe after delivery, because the lungs do not grow as big as they should (pulmonary hypoplasia), the blood pressure in the lungs may remain high (pulmonary hypertension), and the heart is compressed and may have to work harder than normal (cardiac dysfunction).
CDH occurs in 1 in 2500 babies and there are only 1600 babies born in the United States with CDH each year. The size and location of the hole in the diaphragm is different for each baby and can impact your baby’s need for medical support after birth. This is a rare and complex disorder, and it is necessary to have an experienced and dedicated team to care for you and your baby. For us to best prepare for the care your baby will need when he or she is born, additional testing is crucial.
Infants with CDH have challenges with their lungs, heart, and intestines
The abdominal organs that are in the chest while your baby is developing cause pressure on the lungs and heart and can impact the intestines themselves in the following common ways:
Lungs:
- The lungs are smaller than those in a baby without CDH. This is called pulmonary hypoplasia.
- ◦ Your baby will need help breathing right after they are born. With time, most babies with CDH can breathe on their own without oxygen support.
- ◦ A consistent management approach that is tailored to your baby’s individual needs and focuses on safe, gentle breathing support is crucial to help your baby’s lungs continue to grow and develop after birth.
- The blood pressure in the lungs is higher than it should be.
- ◦ This is called pulmonary hypertension and can make it difficult for your baby to get enough oxygen into their bloodstream.
- ◦ We have several medications and therapies that we can use to ensure the high blood pressure in your baby’s lungs is controlled.
Heart:
- Some of the structures in the heart are smaller than they should be.
- ◦ The pressure placed on the heart by the abdominal organs in the chest can cause the chamber of the heart responsible for pumping blood to the body to be smaller than normal.
- ◦ With appropriate support after the hernia is repaired, your baby’s heart will grow to a normal size over time.
- The normal changes that occur during and after birth can cause the heart of a baby with CDH to function poorly, which can make your baby very sick.
- ◦ In the first two hours after your baby is born, an echocardiogram, or ultrasound of the heart, will be performed to help your baby’s team decide how best to support your baby.
- ◦ Our evidenced-based protocol focuses on rapid support of your baby’s individualized needs. The St. Louis Children’s Hospital CDH team understands that frequent evaluations and aggressive management of decreased heart function in the baby with CDH has been shown to improve survival rates.
Intestines:
- Intestinal development and function are abnormal
- ◦ It will take several days after your baby’s stomach and intestines are returned to his or her abdomen for bowel function to return.
- ◦ Feeding intolerance and gastroesophageal reflux is common in babies with CDH.
- Tailored, comprehensive nutritional support is crucial to the survival of babies with CDH
- ◦ Our CDH team’s dietician and NICU lactation consultants will ensure your baby receive the proper nutrition throughout the stay, including helping you pump and store breastmilk after delivery.
- ◦ In the first few days to weeks after delivery, your baby will be unable to eat breastmilk. Instead, intravenous (IV) nutrition will be started in the days after birth to ensure your baby has the energy to heal and grow.
Causes of CDH
The diaphragm, which is the thin muscle that supports breathing and separates the abdomen from the chest, forms between weeks 4 and 12 in pregnancy. The esophagus (tube that brings food and water from the throat to the stomach) and the intestines also form during this time. Rarely, the diaphragm does not form as it should, and a congenital diaphragmatic hernia occurs.
There are two types of congenital diaphragmatic hernia. The most common is called Bochdalek hernia, which occurs when the part of the diaphragm closest to your baby’s back and side does not completely close, allowing abdominal organs to reside in the chest. Bochdalek hernia occurs in 80-90% of CDH cases. The other type, Morgagni hernia, is much less common (1 in 50 cases of CDH each year) and occurs when the tendon that should form in the middle of the diaphragm doesn’t develop as it should. This leaves a hole in the part of the diaphragm closest to your baby’s chest. In both cases, the diaphragm and digestive tract don’t form as they are supposed to. The heart and lungs are affected, as well.
Diaphragmatic hernia can be caused by many factors, including genetics or something in the environment. Your baby will be evaluated by our pediatric genetics doctors to try and find a genetic cause of your baby’s CDH. Often, we do not find out why the diaphragm did not close.
Diagnosis of CDH
Approximately 3/4 of all cases of congenital diaphragmatic hernia are diagnosed before birth, frequently at the 20-week anatomy scan. This will prompt many more tests, such as additional specialized ultrasound, genetic testing, fetal MRI, and a fetal echocardiogram. Although the defect may seem small on the initial ultrasound, CDH can evolve over pregnancy and follow-up tests performed and interpreted by specialists experienced in the care of babies with CDH before, during, and after delivery are crucial to your baby’s survival after birth.
If your unborn baby has been diagnosed with CDH, please request a referral to our Fetal Care Center. At your appointment, you will undergo a detailed fetal ultrasound, counseling with an expert in fetal diagnosis and pregnancy care, a fetal MRI, a safe imaging scan that provides far more accurate information about your growing baby than an ultrasound. You will then meet the Medical Director for the NICU CDH Team who will partner with you to understand your baby’s unique needs, the challenges they may face, and how we can help your baby live a happy, healthy life.
Occasionally, CDH is not diagnosed until after birth. Your baby may have had difficulty breathing after birth, needing oxygen support. Transfer to a newborn intensive care unit with experience in providing specialized care to infants with CDH is important to ensure best outcomes. Saint Louis Children’s Hospital Newborn Transport Team is experienced in caring for CDH patients who are born at hospitals other than Barnes Jewish and bringing them safely to the NICU at Saint Louis Children’s Hospital.
Treatment for CDH
Research shows that babies with CDH have the best chance of survival when they are born at a hospital like our Women & Infants Center that specializes in high-risk pregnancies and has immediate access to advanced care in a Level IV newborn intensive care unit (NICU). Your baby’s treatment may include the following:
Newborn intensive care unit (NICU): Babies with this condition need care in a Level IV NICU, which is equipped to provide a high-level of specialized care. These babies cannot breathe well on their own because their lungs are not fully developed. Most babies will need to use a breathing machine (mechanical ventilator). This can help them breathe. They may also need medicines to help support their blood pression and to help them breathe. Learn more about the CDH care provided in our St. Louis Children's Hospital NICU.
Extracorporeal membrane oxygenation (ECMO): Some babies with severe breathing or heart problems need to be put on a heart/lung bypass machine (ECMO). ECMO takes over the role of the baby’s heart and lung while they are too sick to do it on their own. It puts oxygen in your baby’s bloodstream and pumps blood to your baby’s body. ECMO may be used temporarily. Your baby may need it until his or her condition gets better.
Surgery: Once your baby is in good enough condition, he or she will need to have surgery to fix the diaphragmatic hernia. Your baby’s surgeon will move your baby’s stomach, intestine, and other abdominal organs from the chest cavity back to the abdominal cavity. The surgeon will also fix the hole in your baby’s diaphragm. If the hole is small, the surgeon will be able to sew it closed. If the hole is large, the surgeon may need to use a special material to patch the hole in the diaphragm. Your baby’s surgeon will speak to you at length and answer any questions you may have before the procedure takes place.
After Surgery: Your baby will need to stay in the NICU after surgery. This is because your baby’s lungs will still be underdeveloped, and the blood pressure in your baby’s lungs will be high. Your child will still need breathing support for days to weeks after surgery. After your baby is done using the breathing machine, he or she may still need oxygen or medicine to help with breathing. Your child may need this for weeks, months, or, in rare cases, years.
Once your baby is more stable, he or she will receive tiny amounts of breastmilk through a feeding tube. Babies with CDH tend to tolerate maternal breast milk the best. Our CDH team dietician and NICU lactation consultants are available to help you pump and store breastmilk after delivery. If you cannot provide breast milk or do not wish to, the team can discuss donor breast milk or alternative nutrition sources.
We will discuss your feeding preferences for your baby. Babies with CDH can be sensitive to formula, so we highly recommend feeding them breastmilk that you have pumped. We have a full team of lactation consultants and pumping equipment in the NICU to help you produce breastmilk if that is your choice. We recognize that providing breastmilk is not always feasible or the best choice for you; if you choose not to breastfeed or are unable to pump breastmilk, we can use donor breastmilk as a safe alternative. For many children with CDH, eating can be challenging. Learn more.
Follow-Up Care:  CDH babies can experience long-term health problems. It is important to have a multidisciplinary clinic care and follow your child as they grow so they can thrive. Our St. Louis Children’s Hospital CDH clinic allows your child to have coordinated care between neonatologists, pulmonologists, and neurologists specializing in CDH care. Children with CDH also have access to dieticians, occupational therapists, physical therapist, and speech therapists in the CDH Clinic. An appointment will be scheduled for the month after your baby is discharged in this outpatient clinic, and these specialty services will continue to be available to your child until they are teenagers. Many of these medical providers are the ones who cared for your child in our NICU.
CDH babies can experience long-term health problems. It is important to have a multidisciplinary clinic care and follow your child as they grow so they can thrive. Our St. Louis Children’s Hospital CDH clinic allows your child to have coordinated care between neonatologists, pulmonologists, and neurologists specializing in CDH care. Children with CDH also have access to dieticians, occupational therapists, physical therapist, and speech therapists in the CDH Clinic. An appointment will be scheduled for the month after your baby is discharged in this outpatient clinic, and these specialty services will continue to be available to your child until they are teenagers. Many of these medical providers are the ones who cared for your child in our NICU.
If your unborn baby has been diagnosed with CDH, please request a referral to our Fetal Care Center.










