What is Pediatric Liver Cancer?
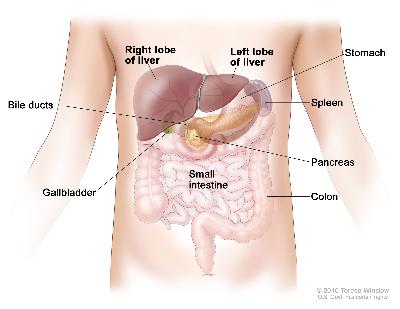
Childhood liver cancer is a disease in which malignant (cancer) cells form in the tissues of the liver. The liver is one of the largest organs in the body. It has four lobes and fills the upper right side of the abdomen inside the rib cage. The liver has many important functions, including:
- Filtering harmful substances from the blood so they can be passed from the body in stools and urine.
- Making bile to help digest fats from food.
- Storing glycogen (sugar), which the body uses for energy.
For more information regarding liver cancer services in St. Louis, please call 314.454.5437 or 800.678.5437 or email us.
Liver cancer is rare in children and adolescents (teenagers). There are two main types of childhood liver cancer:
- Hepatoblastoma: A type of liver cancer that usually does not spread outside the liver. This type usually affects children younger than 3 years old.
- Hepatocellular carcinoma: A type of liver cancer that often spreads to other places in the body. This type usually affects children older than 14 years old.
The treatment of two less common types of childhood liver cancer are:
- Undifferentiated embryonal sarcoma of the liver (UESL): The third most common liver cancer in children and adolescents. It usually occurs in children between the ages of 5 and 10 years.
- Infantile choriocarcinoma of the liver: A very rare tumor that appears to start in the placenta and spreads to the fetus. The tumor is usually found during the first few months of life.
For more information or to request an appointment with a pediatric oncologist at St. Louis Children's Hospital, call 314.454.5437 or 800.678.5437 or email us.
Risk Factors for Liver Cancer
Certain diseases and disorders can increase the risk of developing childhood liver cancer. Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. If you think your child may be at risk, you should discuss with their doctor. Risk factors for hepatoblastoma include the following:
- Being male.
- Having familial adenomatous polyposis (FAP).
- Having Beckwith-Wiedemann syndrome.
- Having had a very low weight at birth.
Risk factors for hepatocellular carcinoma include the following:
- Being male.
- Having hepatitis B or hepatitis C. The risk is greatest when the virus is passed from mother to child at birth.
- Having liver damage caused by certain diseases, such as biliary cirrhosis or tyrosinemia.
Signs and Symptoms of Pediatric Liver Cancer
Symptoms are more common after the tumor becomes large. Other conditions can cause the same symptoms. A doctor should be consulted if any of the following problems occur:
- A painless lump in the abdomen.
- Swelling or pain in the abdomen.
- Weight loss for no known reason.
- Loss of appetite.
- Early puberty in boys.
- Nausea and vomiting.
Pediatric Liver Cancer Diagnosis
Tests that examine the liver and the blood are used to detect and diagnose childhood liver cancer. The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Serum tumor marker test: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The blood of children who have liver cancer may have increased amounts of a protein called alpha-fetoprotein (AFP) or a hormone called beta-human chorionic gonadotropin (β-hCG). Other cancers and certain noncancerous conditions, including cirrhosis and hepatitis, may also increase AFP levels.
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells, white blood cells, and platelets.
- The amount of hemoglobin (the protein that carries oxygen)in the red blood cells.
- The portion of the blood sample made up of red blood cells.
- Liver function tests: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by the liver. A higher than normal amount of a substance can be a sign of liver cancer.
- Abdominal x-ray: An x-ray of the organs in the abdomen. An x-ray is a type of energy beam that can go through the body onto film, making a picture of areas inside the body.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. In childhood liver cancer, a CT scan of the chest and abdomen is usually done.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer. The sample may be taken during surgery to remove or view the tumor. A pathologist views the sample under a microscope to determine the type of liver cancer.
For more information or to request an appointment with a pediatric oncologist at St. Louis Children's Hospital, call 314.454.5437 or 800.678.5437 or email us.
Treatment of Pediatric Liver Cancer
Certain factors affect prognosis (chance of recovery) and treatment options. The chance of recovery and treatment options depend on the following:
- The stage of the cancer (the size of the tumor, whether it affects part or all of the liver, and whether it has spread to other places in the body, such as the lungs).
- Whether the cancer can be removed completely by surgery.
- The type of liver cancer.
- Whether the cancer has just been diagnosed or has recurred.
Prognosis may also depend on:
- Certain features of the cancer cell (how it looks under a microscope).
- Whether the AFP blood levels go down after chemotherapy begins.
Childhood liver cancer may be cured if the tumor is small and can be completely removed by surgery. Complete removal is possible more often for hepatoblastoma than for hepatocellular carcinoma.
Stages of Childhood Liver Cancer
After childhood liver cancer has been diagnosed, tests are done to find out if cancer cells have spread within the liver or to other parts of the body.
The process used to find out if cancer has spread within the liver or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment.
The following tests and procedures may be used in the staging process:
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
- Surgery: An operation will be done to look at or remove the tumor. Tissues removed during surgery will be checked by a pathologist.
Two staging systems are used for childhood liver cancer:
- Presurgical (before surgery) staging: The stage is based on where the tumor has spread within the four parts (sections) of the liver, as shown by imaging procedures such as MRI or CT. This staging system is called PRETEXT.
- Postsurgical (after surgery) staging: The stage is based on the amount of tumor that remains after the patient has had surgery to look at or remove the tumor.
The liver is divided into four vertical sections. Before surgery, the following stages are used before surgery:
PRETEXT Stage 1
.jpeg)
In stage 1, the cancer is found in one section of the liver. Three sections of the liver that are next to each other do not have cancer in them.
PRETEXT Stage 2
.jpeg)
In stage 2, cancer is found in one or two sections of the liver. Two sections of the liver that are next to each other do not have cancer in them.
PRETEXT Stage 3
.jpeg)
In stage 3, one of the following is true:
- Cancer is found in three sections of the liver and one section does not have cancer.
- Cancer is found in two sections of the liver and two sections that are not next to each other do not have cancer in them.
PRETEXT Stage 4
.jpeg)
In stage 4, cancer is found in all four sections of the liver.
For more information or to request an appointment with a pediatric oncologist at St. Louis Children's Hospital, call 314.454.5437 or 800.678.5437 or email us.
After Liver Cancer Surgery
The following stages are used after surgery:
Stage I
In stage I, the tumor was in the liver only and all of the cancer was removed by surgery.
Stage II
In stage II, the tumor was in the liver only and all of the cancer that can be seen without a microscope was removed by surgery. A small amount of cancer remains in the liver, but it can be seen only with a microscope, or the tumor cells may have spilled into the abdomen before surgery or during surgery.
Stage III
In stage III:
- The tumor cannot be removed by surgery; or
- Cancer that can be seen without a microscope remains after surgery; or
- The cancer has spread to nearby lymph nodes.
Stage IV
In stage IV, the cancer has spread to other parts of the body. There are three ways that cancer spreads in the body:
- Through tissue: Cancer invades the surrounding normal tissue.
- Through the lymph system: Cancer invades the lymph system and travels through the lymph vessels to other places in the body.
- Through the blood: Cancer invades the veins and capillaries and travels through the blood to other places in the body.
When cancer cells break away from the primary (original) tumor and travel through the lymph or blood to other places in the body, another (secondary) tumor may form. This process is called metastasis. The secondary (metastatic) tumor is the same type of cancer as the primary tumor. For example, if breast cancer spreads to the bones, the cancer cells in the bones are actually breast cancer cells. The disease is metastatic breast cancer, not bone cancer.
Recurrent Childhood Liver Cancer
Recurrent pediatric liver cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back in the liver or in other parts of the body.
Treatment Option Overview
Different types of treatments are available for children with liver cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other doctors who are experts in treating children with liver cancer and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery. Other specialists may include the following:
- Radiation oncologist
- Pediatric nurse specialist
- Rehabilitation specialist
- Psychologist
- Social worker
For more information or to request an appointment with a pediatric oncologist at St. Louis Children's Hospital, call 314.454.5437 or 800.678.5437 or email us.
Side Effects of Cancer Treatments
Side effects from cancer treatment that begin during or after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include:
- Physical problems
- Changes in mood, feelings, thinking, learning, or memory
- Second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the effects cancer treatment can have on your child. (See the PDQ summary on Late Effects of Treatment for Childhood Cancer for more information).
Pediatric Liver Cancer Surgery
When possible, the cancer is removed by surgery. Five types of standard treatment are used:
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue, such as carcinoma in situ. This type of treatment is also called cryotherapy. The doctor may use ultrasound to guide the instrument.
- Partial hepatectomy: Removal of the part of the liver where cancer is found. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with a small amount of normal tissue around it.
- Total hepatectomy and liver transplant: Removal of the entire liver and replacement with a healthy liver from a donor. A liver transplant may be possible when cancer has not spread beyond the liver and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
- Resection of metastases: Surgery to remove cancer that has spread outside of the liver, such as to nearby tissues, the lungs, or the brain.
Some of the factors that affect the type of surgery used include the following:
- The PRETEXT stage (stage of the cancer before surgery).
- The size of the primary tumor.
- Whether there is more than one tumor in the liver.
- Whether the cancer has spread to blood vessels.
- The level of alpha-fetoprotein in the blood.
- Whether the tumor can be shrunk by chemotherapy so that it can be removed by surgery.
- Whether a liver transplant is needed.
Chemotherapy is sometimes given before surgery, to shrink the tumor and make it easier to remove. This is called neoadjuvant therapy. Even if the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Watchful Waiting
Watchful waiting is closely monitoring a patient’s condition without giving any treatment until symptoms appear or change.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Chemoembolization of the hepatic artery (the main artery that supplies blood to the liver) is a type of regional chemotherapy used to treat childhood liver cancer. The anticancer drug is injected into the hepatic artery through a catheter (thin tube). The drug is mixed with a substance that blocks the artery, cutting off blood flow to the tumor. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on the substance used to block the artery. The tumor is prevented from getting the oxygen and nutrients it needs to grow. The liver continues to receive blood from the hepatic portal vein, which carries blood from the stomach and intestine.
Treatment using more than one anticancer drug is called combination chemotherapy. The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Radiation Therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy. External radiation therapy uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer. The way the radiation therapy is given depends on the type and stage of the cancer being treated.
Percutaneous Ethanol Injection
Percutaneous ethanol injection is a cancer treatment in which a small needle is used to inject ethanol (alcohol) directly into a tumor to kill cancer cells.
For more information regarding liver cancer services in St. Louis, please call 314.454.5437 or 800.678.5437 or email us.










