By Pam McGrath
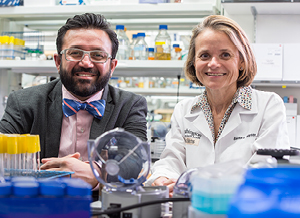 Washington University neonatologist Barbara Warner, MD, co-director of the Fetal Care Center—a partnership between St. Louis Children’s Hospital, Barnes-Jewish Hospital and Washington University Physicians—begins a discussion about antibiotic use in premature infants with an important caveat: Antibiotics have probably saved more lives than they have harmed. That said, she and her colleagues are working toward a better understanding of how best to use antibiotics in premature infants. Their goal is to ensure that the medications designed to combat infections while these tiny patients are in the newborn intensive care unit (NICU) don’t compromise their ability to stave off illness when they are older.
Washington University neonatologist Barbara Warner, MD, co-director of the Fetal Care Center—a partnership between St. Louis Children’s Hospital, Barnes-Jewish Hospital and Washington University Physicians—begins a discussion about antibiotic use in premature infants with an important caveat: Antibiotics have probably saved more lives than they have harmed. That said, she and her colleagues are working toward a better understanding of how best to use antibiotics in premature infants. Their goal is to ensure that the medications designed to combat infections while these tiny patients are in the newborn intensive care unit (NICU) don’t compromise their ability to stave off illness when they are older.
THE ANTIBIOTIC CONUNDRUM
Within the past decade, the medical community has come to understand that there is a cost to using the miracle drugs making up the antibiotic arsenal, especially in the case of broad-spectrum antibiotics—those designed to act against a wide range of disease-causing bacteria.
“The most notable cost is the emergence of antibiotic-resistant organisms,” says Dr. Warner. “If these continue to develop, there’s the potential for us eventually entering an era where there are no drugs available to treat infections like methicillin-resistant Staphylococcus aureus or necrotizing entercolitis.”
This is particularly worrisome in the case of premature infants. Antibiotics are a mainstay of medical therapy for this at-risk population and essential to maintaining a low mortality rate.
“The challenge with babies in the NICU is that the symptomatology for sepsis overlaps considerably with that of being preterm,” explains Dr. Warner. “In both cases, these babies may be breathing fast, have trouble breathing, or experience apnea. This may be due to infection or to their lungs not being fully developed.”
Because of the difficulty diagnosing infections in these newborns, in the past the practice was to prescribe antibiotics to all premature infants. That approach is no longer an automatic “go to” in the Children’s Hospital NICU.
A CHANGING PHILOSOPHY
Thanks to large epidemiologic studies that have identified risk factors for infection in both term and preterm infants, neonatologists now have tools to make better decisions regarding the use of antibiotics.
“If the mother of a full-term infant had no labor, no rupture of membranes and no sign of infection but the baby is breathing fast and needs a bit of oxygen then, depending on the degree of severity of illness, we now feel more comfortable watching that baby a little longer and looking at blood tests before deciding on antibiotic use,” says Dr. Warner. “Although a preterm infant with a similar repertoire of symptoms is more likely to be put on antibiotics, we are still more comfortable looking closely at those risk factors before prescribing these medications.”
When antibiotics are needed, careful decisions are made regarding the type chosen. Studies have shown that broad-spectrum antibiotics increase the possibility for infants to develop resistant organisms that are difficult to treat. In the NICU, older, narrow-spectrum antibiotics like ampicillin and gentamicin are used whenever possible, rather than drugs such as the broader-spectrum meropenem.
“Whenever possible, more powerful antibiotics should be held in reserve in case other issues arise,” says Jason Newland, MD, MEd, Washington University pediatric infectious diseases physician at St. Louis Children’s Hospital, and director of the hospital’s Antimicrobial Stewardship Program. Begun two years ago, the program’s team members review and monitor antibiotic use within the hospital on a daily basis. “Consideration also needs to be given to the negative consequences associated with certain antibiotics, such as development of a fungal infection in the blood.”
Another important aspect of the NICU’s approach to antibiotics is establishing a “hard stop” to their use. This is another instance in which the Antimicrobial Stewardship Program plays an important role in patient care.
“Before the drawbacks of antibiotics were realized, a prescribed course of one week sometimes extended to 10 days without much concern about it,” says Dr. Warner. “Dr. Newland and his team help to ensure a stop date is established and followed.”
She adds, “We also have more tolerance for discontinuing antibiotics prior to a stop date. If a baby doesn’t show other signs of infection, the blood tests are reassuring, and the problems likely stem from premature lungs, we are often comfortable discontinuing antibiotics within just a few days.”
RESEARCHING ANTIBIOTICS’ EFFECTS ON PREMATURE INFANTS’ GUT BACTERIA
In recent years, the gut microbiome has emerged as a vital player in human health, affecting factors as diverse as nutritional status, bone development and immune function. Dr. Warner has worked with Gautam Dantas, PhD, professor of pathology and immunology at Washington University School of Medicine, and other colleagues to determine the extent of antibiotic resistance in the gut bacteria of premature infants. Their findings showed that the microbes colonizing the gastrointestinal tracts of babies born prematurely are not health-promoting or even benign organisms, but close relatives of bacteria known to cause hospital-acquired infections, including Escherichia coli (E. coli), Klebsiella and Enterobacter.
“Our study demonstrated that even well-studied bacteria—the ones we know cause disease or their close relatives—have many genes associated with antibiotic resistance that had not been characterized before,” says Dr. Dantas. “Premature babies do not always get bacterial infections that need treatment, but we have known for a long time they are at higher risk for infection than babies born full term. Now, we know that preterm-infant guts are attracting exactly the wrong kinds of bacteria.”
In general, research from this and other groups suggests it is better to have a high diversity of bacterial species living in the gut. Compared with babies born full term, preterm infants were found to have 10-fold fewer species of bacteria colonizing the gut. And among the preterm babies, those receiving the most antibiotics showed the least species diversity. Giving breast milk was associated with increased bacterial diversity, as was each baby’s increasing age, perhaps simply from having more time for exposure.
LESSONS FOR THE PEDIATRIC COMMUNITY
Based on the research findings from the Dantas laboratory and her daily experience dealing with antibiotics in an at-risk population, Dr. Warner says there are two lessons for pediatricians.
“First, antibiotics are clearly life-saving, but they do come with a cost—short term in the development of antibiotic resistance and long term in regard to child health,” she says. “Second, narrow the spectrum of antibiotics as appropriate for the clinical condition and monitor their use carefully. This kind of thoughtful attention is vital to the medical community’s effort in combating antibiotic resistance in new generations.”
For more information about antibiotic use in at-risk populations, call Children’s Direct at 800.678.HELP (4357).