by Pam McGrath
 At age 14, Madeline Rauh was an exceptional student and talented competitive swimmer. According to her mom, Julie, her daughter was seldom sick and, other than routine physical exams, rarely needed to see her pediatrician.
At age 14, Madeline Rauh was an exceptional student and talented competitive swimmer. According to her mom, Julie, her daughter was seldom sick and, other than routine physical exams, rarely needed to see her pediatrician.
Then in April 2015 Madeline began coughing and feeling fatigued, symptoms that persisted over two weeks. She tested positive for strep throat but negative for mononucleosis, so her pediatrician prescribed antibiotics. When she continued to feel poorly her parents took her to the emergency department at St. Louis Children’s Hospital. There a blood test uncovered something alarming—Madeline was in kidney failure. Her creatinine, which for someone her age should have been .6 to 1, was 24. A kidney biopsy showed that Madeline had antiglomerular basement membrane (anti-GBM) antibody disease, also known as Goodpasture’s syndrome.
“Anti-GBM is a rare autoimmune disorder in which a person’s immune system begins attacking proteins in the glomerular basement membrane, the middle layer of the kidney’s filtration barrier,” says Washington University physician Vikas Dharnidharka, MD, MPH, division chief of pediatric nephrology. “This is a poorly defined immune system abnormality that may be triggered by a cold or infection. Most often it occurs in teens and young adults in their 20s.”
Anti-GBM antibodies also may attack proteins in the lungs, which sometimes results in patients coughing up blood. For Madeline, only her kidneys were affected.
“If diagnosed early enough, kidney damage in some anti-GBM patients can be reversed. However, this disease progresses rapidly and diagnosis can be delayed when symptoms are relatively mild, as in Madeline’s case,” says Washington University physician S. Paul Hmiel, MD, PhD, medical director, pediatric kidney transplant.
In a matter of a few days Julie and her husband, Nathan, went from having a healthy, rarely sick daughter to watching her be placed on hemodialysis. “It was a huge shock. We hoped her kidneys would recover, but within a month’s time we began to understand that wasn’t going to happen,” says Julie. “This came so much out of the blue we felt the doctors were giving us some time to cope with the idea of our daughter needing to be on dialysis permanently or undergoing a transplant. That’s when we began approaching Madeline’s illness day by day.”
After remaining on hemodialysis for about a month, Madeline switched to home-based peritoneal dialysis. She needed to continue dialysis for the next six months to ensure the anti-GBM didn’t affect her lungs or other organ systems.
“Although her dad immediately volunteered to be Madeline’s living donor, we needed to make sure her immune system was suppressed to the point where it wouldn’t attack a newly transplanted kidney,” says Dr. Hmiel.
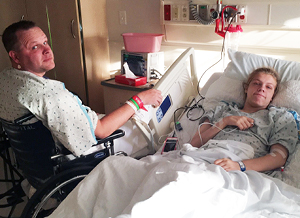
On June 15, 2016, 14 months after Madeline’s diagnosis, Nathan donated a kidney to his daughter. “It’s hard to describe the feeling when you realize everything is going to work out,” he says.
According to Madeline’s transplant surgeon, Washington University physician Jason Wellen, MD, Nathan’s donated kidney was the best possible option for his daughter. “His kidney already was a 50 percent match to Madeline, which reduced the chance of rejection, and we were able to transplant it into Madeline within about 20 minutes. That usually means the kidney begins to function more quickly and lasts much longer than a deceased kidney donation,” he says.
Madeline’s health improved immediately and as soon as receiving clearance from her physicians, she returned to her high school swim team and improved her time in the butterfly and 200 individual medley by eight seconds. She finished sixth at the Missouri State High School Activities Association swimming competition in both her junior and senior years, as well as winning gold medals at the Transplant Games of America in Salt Lake City following her junior year.
“These successes made me look back and feel proud of how far I’d come and how my dad helped me get to that point,” says Madeline.
According to her kidney transplant coordinator, Madeline was an exceptional transplant patient, especially in light of her being a teenager.
“Teens often don’t follow the strict medication regimen that’s required after a transplant, but Madeline took learning about her meds and taking responsibility for them quite seriously,” says Michelle Rozier, RN, BSN. “And her parents provided her support while at the same time allowing her to be successful and independent.”
That allowed independence included the Rauhs helping  Madeline move to Savannah, Georgia, this fall to attend the Savannah College of Art and Design. She’s now responsible for refilling her prescriptions, scheduling monthly lab tests, taking meds on time—and then texting her mom to let her know that she has. A talented artist and animator, after college Madeline may set her sights on a position at Disney or Pixar, or perhaps a small, independent animation studio. Whatever she chooses, she’ll approach her future with the even-tempered determination and persistence that brought her through a rare medical crisis.
Madeline move to Savannah, Georgia, this fall to attend the Savannah College of Art and Design. She’s now responsible for refilling her prescriptions, scheduling monthly lab tests, taking meds on time—and then texting her mom to let her know that she has. A talented artist and animator, after college Madeline may set her sights on a position at Disney or Pixar, or perhaps a small, independent animation studio. Whatever she chooses, she’ll approach her future with the even-tempered determination and persistence that brought her through a rare medical crisis.
To speak with a member of the Washington University pediatric kidney transplant team at St. Louis Children’s Hospital, call Children’s Direct at 800.678.HELP (4357).









