As 6-year-old Stacey was getting ready for her bath, she suddenly couldn’t move her left arm. Moments later, the left side of Stacey’s face drooped.
Her mom, Brandy Mitchell, called 911 immediately. At the hospital near their home in Aledo, Illinois, a CT scan showed Stacey had a stroke. She was quickly transferred to an Iowa children’s hospital where doctors conducted an angiogram and determined Stacey had moyamoya disease.
Moyamoya is a rare disease in which the arteries that supply blood to the brain become narrowed and limit blood flow to the brain. Moyamoya progresses over time and puts patients at risk for stroke.
By the time Stacey was diagnosed with moyamoya, she had already had two strokes at home. She was given medication after diagnosis but she had two more strokes over the next two weeks. Doctors were puzzled and knew St. Louis Children’s Hospital could offer more expertise in moyamoya. So Stacey was transferred to St. Louis under the care of Kristin Guilliams, MD, a Washington University pediatric neurologist and critical care physician at St. Louis Children’s Hospital.
A Specialized Program for Comprehensive Care
St. Louis Children’s Hospital is a referral center for moyamoya and follows about 20 patients with the disease. The Moyamoya Program at Children’s includes a multidisciplinary team of pediatric neurosurgeons, neurologists, pediatricians, neuroradiologists, anesthesiologists, and physicians who work together to protect the brains and development of children with moyamoya.
Dr. Guilliams’ first challenge was to determine why Stacey continued to have strokes.
“Unfortunately, a stroke is the most common way we discover someone has moyamoya,” Dr. Guilliams explain. “Occasionally we will find moyamoya when we’re obtaining brain imaging for something else.”
Moyamoya often doesn’t cause any problems until early grade school age, which is a time of tremendous brain growth. “As the body and blood vessels grow, the brain needs more blood flow,” Dr. Guilliams says. “Moyamoya narrows the blood vessels. In Stacey’s case, she was just recovering from a gastrointestinal illness and was dehydrated, which decreased her blood pressure. It was the perfect storm at the time of her first stroke. But Stacey also presented an extra challenge because she continued to have strokes even after she received rehydration.”
Two of her strokes occurred during her sleep, as her stroke symptoms were noted in the morning upon awakening. After being monitored during sleep at Children’s, the team discovered Stacey’s blood pressure dropped more than 20 percent during sleep before the team intervened to prevent her blood pressure from going lower. Having a low blood pressure for hours during sleep likely led to her strokes during sleep, Dr. Guilliams explains. Typically when blood pressure decreases, blood vessels can dilate to allow more blood flow. But because moyamoya causes the blood vessels to narrow, they can’t dilate enough to keep adequate blood flow to the brain.
Dr. Guilliams says the goal was to get Stacey to surgery as soon as it was safe to do so. Jennifer Strahle, MD, a Washington University pediatric neurosurgeon who co-leads the Moyamoya Program at St. Louis Children’s Hospital, had to find the optimum timing and the optimum procedure for Stacey.
The Right Procedure with the Right Team
There are two types of revascularization to treat moyamoya: direct or indirect. “With direct revascularization, surgeons redirect a superficial blood vessel and graft it into the moyamoya vessel past the area of narrowing to provide blood flow distal to the narrowing,” Dr. Guilliams says. “However, the concern is a sudden increase in blood flow that could cause reperfusion injury or bleeding, particularly after a large stroke. With indirect revascularization, surgeons lay a blood vessel on the surface of the brain, which promotes blood vessel growth from the outside in. The brain then develops an alternate blood flow naturally. The challenge is that it takes time to grow the blood vessel—several months to a year.”
Neurosurgeons at St. Louis Children’s Hospital performed the indirect revascularization procedure on Stacey March 15, 2018, about two months after her initial strokes at home. During surgery, she received continuous EEG monitoring. Rejean Guerriero, DO, a neurocritical care epileptologist, sat in the OR to monitor the electrical activity in her brain.
“What’s fantastic about our pediatric stroke program is having the whole team involved to pull off a successful surgery,” Dr. Guilliams says. “It takes a village, including stroke specialists, pediatric neurointerventional radiologists, a pediatric neurosurgeon trained in revascularization surgery such as Dr. Strahle, epileptologists and the OR and ICU EEG monitoring service that few centers have.”
In addition, Children’s has a neurorehabilitation program with therapists who are experienced in pediatric stroke and rehabilitation.
“Many people don’t realize kids can have strokes,” Dr. Guilliams says. “But stroke is one of the top 10 reasons children die in the U.S. One of the reasons we have a stroke program is that a dedicated pediatric stroke program can literally save a child’s life. The kids are a big motivator for our team to work hard to research, understand and treat pediatric stroke.”
The stroke program at St. Louis Children’s Hospital offers hyperacute stroke treatment, including tPA, the clot-busting drug, and thrombectomy, clot retrieval.
Less than two years ago, St. Louis Children’s Hospital established a Neurocritical Care Clinic follow-up program. There is only one other similarly structured clinic like this in the country currently.
“After children have a stroke or brain injury, they come back to our neurocritical care follow-up bridge clinic so we can check on things that influence recovery such as school, sleep, and headaches,” Dr. Guilliams says. “They also all see a neuropsychologist, who evaluates them for learning or cognitive deficits as part of the clinic visit. We have found that 80 percent of kids leave the visit with new recommendations related to school, therapies and/or medications. It’s exciting to offer these improvements but also sobering to realize how much we had not been doing and many issues, such as successful return to school, had been falling through the cracks or not coming to our attention until they returned for routine follow-up several months later. This clinic is a big benefit to patient care.”
She continues: “We have also helped physicians set up similar care closer to their patients’ homes for patients who travel a long distance for specialized inpatient care, but this can be challenging depending on available community resources.”
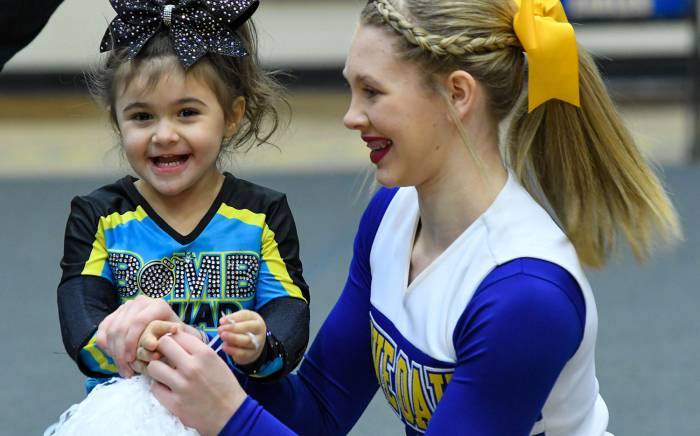
Brandy says Stacey is now bouncing back after her strokes and surgery. “Before surgery, she couldn’t walk. Now she can run. She is getting her range of motion back in her arm, too, and she is gaining strength. She has a harder time focusing and reading, but her short term memory is getting better and Dr. Guilliams reassures me Stacey is on a good track. Stacey has been a rock star—this hasn’t fazed her.”
Brandy says she is grateful for St. Louis Children’s Hospital. “They saved my daughter’s life. They had the knowledge about what to do with compassionate nurses and staff. I had many questions and they answered all of them and were always available to me. They are an incredible group of people.”