Emily Murray knows the value of teamwork and family. The successful businesswoman’s career took her all over the world. Not wanting to go through life without children, she went through a fertility process while living in Chicago and was newly pregnant when COVID-19 made it to the United States.
“I originally planned to transfer to Wichita, Kansas, for work once I was pregnant, but put my things in storage and moved back to St. Louis while everyone was working remotely,” says Emily. “I wanted to be closer to family so they could help once the baby arrived.”
She found an Ob/Gyn at Missouri Baptist Medical Center. Around 36 weeks, Emily went in for a routine ultrasound, and the room quickly went silent.
“I could tell it was a different dynamic,” she says. “When the doctor came in, she said there was a mass on my baby’s brain. They didn’t know what it was, but they wanted me to meet the fetal care team.”
The Fetal Care Center, a partnership among Barnes-Jewish Hospital, St. Louis Children’s Hospital and Washington University Physicians, combines the expertise of specialists in high-risk pregnancy, fetal surgery, and newborn and pediatric care to diagnose, monitor and create a plan of care for both mom and baby before and after birth. Murray is grateful for the team that got the ball rolling and set everything up for her last few weeks of pregnancy.
“It was like a group of superheroes coming into action to save the day,” she says.
A detailed and extensive ultrasound showed the mass in the baby’s brain, and after weighing the options, the fetal care team recommended that Murray deliver her baby by C-section at Barnes-Jewish Hospital on Nov. 30, 2020, because it directly connects to the St. Louis Children’s Hospital newborn intensive care unit (NICU), which offers the highest level of care available to babies. During the two weeks between the diagnosis and the birth, Emily had several conversations with the team.
“They couldn’t be specific because they didn’t know what my child had,” she says. “All the same, everyone made themselves available — even on weekends. They were there with information and honest when they couldn’t give me direct answers.”
Life in the NICU
Elizabeth Murray was born on Nov. 30, 2020. She started crying right away and was whisked off to the St. Louis Children’s Hospital NICU. It was there that Washington University pediatric neurosurgeon Jennifer Strahle, MD, began her work.
“It’s unusual to diagnose a prenatal tumor,” says Dr. Strahle. “After Elizabeth was born, we learned that she had hydrocephalus and a large brain tumor. The tumor appeared to have a lot of blood vessels and it occupied most of her head.”
The pediatric neuro-oncology team met Elizabeth on Dec. 1. Margaret Shatara, MD, is a Washington University pediatric neuro-oncologist at Siteman Kids at St. Louis Children’s Hospital.
“Fetal brain tumors are very rare, so diagnosis is very challenging,” says Dr. Shatara. “In general, most patients with a brain tumor that develops in utero don’t survive or survive with many challenging co-morbidities.”
Elizabeth underwent a needle biopsy of the tumor on her second day of life, and Dr. Shatara says the biopsy and imaging revealed the tumor was most likely a mature teratoma. A mature teratoma is the most common subtype of a teratoma — a type of germ cell tumor that is usually made up of several different types of tissue, including hair, muscle and bone.
“There was no indication that this (tumor) was becoming malignant, and no chemotherapy or radiotherapy helps with these types of tumors,” Dr. Shatara adds. “Early on, chemotherapy was not recommended, and we monitored her.”
Elizabeth also had hydrocephalus, a buildup of fluid in the ventricles (cavities) deep within the brain. The excess fluid, Dr. Strahle says, put pressure on her brain and needed to be drained. The team placed a shunt to control the buildup of fluid, but Dr. Strahle recommended waiting for a few months before scheduling neurosurgery to remove the tumor.
Following the plan
Emily was able to join her newborn daughter at St. Louis Children’s Hospital after a few days. By the time they left the NICU, mom knew there was a team of specialists dedicated to figuring it all out, including the nurse navigator. She learned who all the players were and their roles within the network. It was comforting to know they all had their own specialties. Emily had a plan when she went home with Elizabeth.
“I was always OK,” says Emily. “At every phase there was a plan, and I felt comfortable with that plan. We didn’t know the long-term future, but we could focus on the plan. The experts across all specialties gave me as much time as I needed. We frequently talked through the different options. I never felt like a decision was made for me, but rather we were always partners in Elizabeth’s care. I truly appreciated how much they respected me.”
Between the needle biopsy at two days and an open biopsy six weeks later, Emily and the team decided to give little Elizabeth two rounds of chemotherapy.
“The hope was that the chemo would act on the excessive blood vessels and would allow for a more complete removal of the tumor,” she explains.
On April 28, 2021, Dr. Strahle and her team at the Brain Tumor Center at Siteman Kids at St. Louis Children’s Hospital performed a nine-hour surgery to remove the tumor.
“We were in the hospital for 10 days,” says Emily. “It was very intense for a couple of days, but the whole team was there for us.”
After recovering from the surgery and subsequent shunt revisions to stabilize her cerebral spinal fluid post-operatively, Elizabeth started physical and occupational therapy at the St. Louis Children’s Hospital Specialty Care Center in west St. Louis County. The ball was now in neurology’s court.
Lindsay Peglar, MD, a Washington University neonatal and pediatric neurologist at St. Louis Children’s Hospital, also met Emily before Elizabeth was born.
“Neurosurgery was the main player in the beginning,” says Dr. Peglar. “Our goal was to support Elizabeth and her family every step of the way. Now that she’s stabilized, our team monitors her development and makes sure she has all the support she needs to continue to thrive.”
Murray and her daughter moved to Wichita in December 2021. The following summer, Elizabeth’s shunt malfunctioned, and she needed to return to St. Louis. It would have been an eight-hour drive with a child who was increasingly lethargic and vomiting, but the St. Louis Children’s Hospital Critical Care Transport Team sent their fixed-wing airplane — funded by the St. Louis Children’s Hospital Foundation — to bring Elizabeth to Children’s for a shunt revision.
“The level of care and attention we receive at every turn is truly above and beyond,” says Emily. “The immense fear that came with seeing my daughter in an emergency health situation was eased by knowing that this team of experts would do whatever it takes to help Elizabeth.”
They return to St. Louis every few months to meet with the team.
“Now when we come back to St. Louis for checkups and tests, it’s a homecoming. The people at Children’s are so invested and it feels so personal,” adds Murray. “My nurse navigator, Amber, is awesome — she schedules all our appointments for the subspecialties when we come to St. Louis in a way that makes the trips smooth and coordinated.”
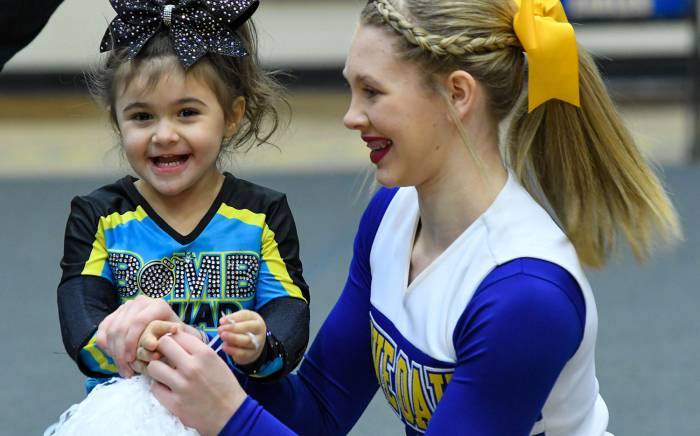
Dr. Peglar diagnosed Elizabeth with right side cerebral palsy in October 2022 but was very happy to see the 2-year-old’s progress. Her fine motor skills are normal for her age and Elizabeth has caught up with her peers in her cognitive ability and language.
“She’s learning how to compensate for that right-side weakness,” Murray says. “She understands everything I say to her, and her communication skills are off the charts.”
Teamwork makes the dream work
The doctors, nurses and hospital staff understand the importance of teamwork. Dr. Shatara says Elizabeth is a testament to using a multidisciplinary approach.
“A brain tumor is not a diagnosis that can be managed by one specialty,” she says. “The disciplines come together each Thursday to discuss newly diagnosed cases or rare/difficult cases. Elizabeth’s case is so rare that it is discussed frequently.”
Dr. Strahle also credits Elizabeth’s mom and family. “Elizabeth has made remarkable recovery and progress for someone with such a large tumor,” says Dr. Strahle. “They put a lot of trust in our teams and our care. It was really a privilege to care for her and be involved with her family. For what we were dealt, Elizabeth’s done really well and continues to improve.”