 Washington University School of Medicine and St. Louis Children’s Hospital have been at the forefront of endocrinology, metabolism and diabetes research since the 1920s. The hospital was the first pediatric institution in the United States to use insulin as a treatment for children with diabetes mellitus. In the 1960s, the pediatric program was among the first in the country to combine patient care, research and training efforts across endocrinology, diabetes and metabolism. The approach has become a standard format at other pediatric academic medical centers.
Washington University School of Medicine and St. Louis Children’s Hospital have been at the forefront of endocrinology, metabolism and diabetes research since the 1920s. The hospital was the first pediatric institution in the United States to use insulin as a treatment for children with diabetes mellitus. In the 1960s, the pediatric program was among the first in the country to combine patient care, research and training efforts across endocrinology, diabetes and metabolism. The approach has become a standard format at other pediatric academic medical centers.
Today, Washington University pediatric endocrinologists at St. Louis Children’s Hospital provide clinical services for children, adolescents and young adults with other forms of the disease. They see an average of 260 new patients with diabetes annually and follow approximately 1,400 patients from states that include Missouri, Illinois, Indiana, Arkansas, Tennessee and Kentucky.
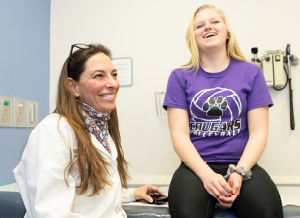
During the past two years, the diabetes program has undergone a reorganization emphasizing four core areas of expertise: clinical care, education, advocacy and community outreach, and research. The team effort was championed by Ana Maria Arbeláez, MD, MSCI, division chief of pediatric endocrinology and diabetes, and Neil White, MD, CDE, director of the pediatric diabetes program.
EXPANDING CLINICAL CARE
“We’ve always delivered outstanding, state-of-the-art clinical care to children with diabetes,” says Dr. White. “Previously that meant patients with type 1 diabetes, but today—in large part due to the obesity epidemic among children and adolescents—we now care for an increasing number of type 2 diabetes patients.”
to children with diabetes,” says Dr. White. “Previously that meant patients with type 1 diabetes, but today—in large part due to the obesity epidemic among children and adolescents—we now care for an increasing number of type 2 diabetes patients.”
The division also has expertise in treating children with other forms of diabetes such as cystic fibrosis-related diabetes through a collaboration with pulmonary medicine. Clinical care and research into rare monogenic types of diabetes such as Wolfram syndrome, neonatal diabetes and MODY are ongoing.
To meet the total needs of the growing patient base, the program has expanded its care team to include—in addition to its 12 pediatric endocrinologists—full-time specialists from pediatric psychology, social work and dietary. It also has increased the number of inpatient and outpatient diabetes educators, pediatric nurse practitioners and clinical educators.
“We are the only pediatric hospital in St. Louis and one of only two in Missouri recognized by the American Diabetes Association for excellence in diabetes education,” says Dr. Arbeláez. “Our multidisciplinary approach ensures our patients receive not only the best medical care but also the knowledge they need to manage their disease and lead healthy lives.”
Easy access to patient care is another hallmark of the program, with clinics at the main hospital; the St. Louis Children’s Hospital Specialty Care Center in west St. Louis County; an outpatient office suite in Arnold, Missouri; and a medical building in Shiloh, Illinois. In addition, patients and their families have 24-hour telephone access to the diabetes team if questions or problems arise.
“Our team is continually working toward bringing cutting-edge drugs and technology to the care of our patients,” says Dr. Arbeláez. “We offer the latest technological options, such as insulin pump therapy and glucose monitoring, to treat the children in the most effective way.”
TRANSITIONING TO ADULT CARE
A new clinical service of significant importance to the diabetes program’s patients provides guidance to young adults 18-21 years old as they move from pediatric to adult care. Called the transition clinic, the first step is for patients to attend “Adulting With Diabetes,” a didactic class that readies them for diabetes self-care management. Then, at their next two clinic appointments, they see a pediatric endocrinologist together with nursing and dietary staff members from the Washington University and Barnes-Jewish Diabetes Center.
“This cooperative interaction between the pediatric and adult diabetes programs is an innovation not seen at many medical centers around the country,” says Dr. Arbeláez. “It brings a continuum of care that encompasses our patients’ first diagnosis through their move to adult care.”
By participating in the transition clinic, patients learn self-management of their disease, from understanding their insulin needs and proper nutrition to knowing how to refill a prescription, make a doctor’s appointment and deal with insurance companies. College-bound patients learn about the effects of alcohol and drugs on their disease, and young women are educated about reproductive health.
“We’ve seen instances of young adults leaving our pediatric clinic with no complications of diabetes, then not seeing an endocrinologist at college, with the consequence of developing kidney disease and eye damage,” says Dr. White. “Our transition clinic is designed to prepare these patients to take over responsibility for their health from their parents.”
EDUCATING PATIENTS, FAMILIES, PROFESSIONALS
The transition clinic is just the newest educational opportunity provided by the pediatric diabetes program to its patients and families. The diabetes program offers comprehensive diabetes care and education with a special emphasis on the use of technology-based tools as well as clinically relevant research to improve patient outcomes. Both beginning and advanced diabetes classes geared toward different age groups are available, as are classes covering self-adjusting insulin dosage, recognizing patterns of blood sugar, dealing with diet and counting carbohydrates, and introduction to insulin pumps and glucose sensors. Beyond the Basics and Survival Skills classes are offered monthly.
“We also are targeting educational opportunities for providers, including community pediatricians, school nurses and teachers,” says Dr. White. “We sponsor a monthly caregiver class so that grandparents, babysitters, nannies—anyone responsible for children with diabetes understands the disease and what to do should complications arise.”
REACHING OUT AND ADVOCATING FOR THE COMMUNITY
One of the most enduring outreach efforts of the pediatric diabetes program is participation by its physicians and nurses in Camp EDI (Exercise, Diet and Insulin), the Ed and Gloria Hirsch Camp for Children with Diabetes. Dr. White has a 35-year history with the camp; for the past 15 years, Washington University pediatric endocrinologist Abby Hollander, MD, has served as the camp’s medical director. Other community efforts include support groups every three months for anyone affected by the disease, including patients, friends, loved ones or caregivers. The program also participates in educational fundraising events with the American Diabetes Association and Juvenile Diabetes Research Foundation, and joins with local vendors to sponsor picnics, movie nights, cooking classes and discussion groups.
“In terms of advocacy, our recent efforts have focused on obtaining better Medicaid coverage for diabetes technology such as insulin pumps and glucose sensors,” says Dr. White. “These are important aspects of diabetes therapy, but state-run insurance in Missouri, Kansas and Illinois provide minimum coverage. It’s important that we work to change this.”
RESEARCH – FROM THE BENCH TO TRANSLATIONAL AND CLINICAL
Washington University and Children’s Hospital have been leaders in the successful completion of many large national and international diabetes studies involving clinical research to improve diabetes management and prevent the disease’s long-term complications. There also is an active interest in clinical studies related to developing and implementing innovative methods of care. These efforts date back to the late Julio Santiago, MD, and Dr. White being among the first in the country to use insulin pumps in the management of patients with type 1 diabetes and their involvement in the landmark Diabetes Control and Complications Trial.
“Other areas of clinical and research expertise include lipid metabolism and bone and mineral metabolism,” says Dr. White. “In addition, over the last few years research interests within the division have branched out into more basic areas of research, including the use and development of animal models to study neuroendocrine regulation and carbohydrate metabolism.”
Taken together, the pediatric diabetes program’s four distinct areas of expertise represent a holistic approach to combating a disease that is of increasing concern in children and teens.
“Our goal is to address our patients’ needs both in the clinical setting and in areas that touch the main components of their lives—school, recreation, family life,” says Dr. Arbeláez. “And we are committed to investigating the basic biology of the disease as well as new treatments that hold promise for bettering the health of our patients.”
To learn more about the diabetes program at St. Louis Children’s Hospital, call Children’s Direct at 800.678.HELP (4357).










